Thyroid and Parathyroid Surgery
Thyroid
Minimal Incision Thyroidectomy
Thyroidectomy is the removal of all or part of your thyroid gland. Your thyroid is a butterfly-shaped gland located at the base of your neck. It produces hormones that regulate every aspect of your metabolism, from your heart rate to how quickly you burn calories.
Thyroidectomy is used to treat thyroid disorders, such as cancer, noncancerous enlargement of the thyroid (goiter) and overactive thyroid (hyperthyroidism).
How much of your thyroid gland is removed during thyroidectomy depends on the reason for surgery. If only a portion is removed (partial thyroidectomy), your thyroid may be able to function normally after surgery. If your entire thyroid is removed (total thyroidectomy), you need daily treatment with thyroid hormone to replace your thyroid’s natural function.
It is estimated that 56,460 men and women (13,250 men and 43,210 women) will be diagnosed with and 1,780 men and women will die of cancer of the thyroid in 2012
The following information is based on NCI’s SEER Cancer Statistics Review2
Thyroid Section
Incidence & Mortality
SEER Incidence
From 2005-2009, the median age at diagnosis for cancer of the thyroid was 50 years of age3
Table I-11 Approximately 1.8% were diagnosed under age 20; 15.5% between 20 and 34; 20.4% between 35 and 44; 24.3% between 45 and 54; 19.0% between 55 and 64; 11.7% between 65 and 74; 5.9% between 75 and 84; and 1.4% 85+ years of age.
The age-adjusted incidence rate was 11.6 per 100,000 men and women per year. These rates are based on cases diagnosed in 2005-2009 from 18 SEER geographic areas.
|
Incidence Rates by Race |
||
|
Race/Ethnicity |
Male |
Female |
| All Races | 5.9 per 100,000 men | 17.3 per 100,000 women |
| White | 6.2 per 100,000 men | 18.3 per 100,000 women |
| Black | 3.3 per 100,000 men | 10.1 per 100,000 women |
| Asian/Pacific Islander | 5.3 per 100,000 men | 17.7 per 100,000 women |
| American Indian/Alaska Native | 3.2 per 100,000 men | 10.9 per 100,000 women |
| Hispanic | 4.2 per 100,000 men | 16.0 per 100,000 women |
US Mortality
From 2005-2009, the median age at death for cancer of the thyroid was 73 years of age4
Approximately 0.1% died under age 20; 0.8% between 20 and 34; 2.2% between 35 and 44; 8.3% between 45 and 54; 16.9% between 55 and 64; 24.7% between 65 and 74; 29.8% between 75 and 84; and 17.3% 85+ years of age.
The age-adjusted death rate was 0.5 per 100,000 men and women per year. These rates are based on patients who died in 2005-2009 in the US.
|
Death Rates by Race |
||
|
Race/Ethnicity |
Male |
Female |
| All Races | 0.5 per 100,000 men | 0.5 per 100,000 women |
| White | 0.5 per 100,000 men | 0.5 per 100,000 women |
| Black | 0.4 per 100,000 men | 0.6 per 100,000 women |
| Asian/Pacific Islander | 0.5 per 100,000 men | 0.8 per 100,000 women |
| Hispanic | 0.5 per 100,000 men | 0.6 per 100,000 women |
Trends in Rates
Trends in rates can be described in many ways. Information for trends over a fixed period of time, for example 1996-2009, can be evaluated by the annual percentage change (APC)
The average annual percent change over several years. The APC is used to measure trends or the change in rates over time. For information on how this is calculated, go to Trend Algortihms in the SEER*Stat Help system. The calculation involves fitting a straight line to the natural logarithm of the data when it is displayed by calendar year. (See Fast Stats for trends over fixed time intervals) . If there is a negative sign before the number, the trend is a decrease; otherwise it is an increase. If there is an asterisk after the APC then the trend was significant, that is, one believes that it is beyond chance, i.e. 95% sure, that the increase or decrease is real over the period 1996-2009. If the trend is not significant, the trend is usually reported as stable or level. Joinpoint analyses
A statistical model for characterizing cancer trends which uses statistical criteria to determine how many times and when the trends in incidence or mortality rates have changed. The results of joinpoint are given as calendar year ranges, and the annual percent change (APC) in the rates over each period can be used over a long period of time to evaluate when changes in the trend have occurred along with the APC which shows how much the trend has changed between each of the joinpoints.
|
The trend in SEER cancer incidence with associated APC(%) for cancer of the thyroid between 1975-2009, All Races |
|||||
|
Male and Female |
Male |
Female |
|||
|
Trend |
Period |
Trend |
Period |
Trend |
Period |
| 6.1 | 1975-1977 | -4.7* | 1975-1980 | 6.7 | 1975-1977 |
| -6.5 | 1977-1980 | 1.9* | 1980-1998 | -5.9 | 1977-1980 |
| 2.4 | 1980-1997 | 5.9* | 1998-2009 | 2.6 | 1980-1997 |
| 6.6 | 1997-2009 | 7.0 | 1997-2009 | ||
|
The joinpoint trend in US cancer mortality with associated APC(%) for cancer of the thyroid between 1975-2009, All Races |
|||||
|
Male and Female |
Male |
Female |
|||
|
Trend |
Period |
Trend |
Period |
Trend |
Period |
| -2.2 | 1975-1988 | -3.2 | 1975-1983 | -2.6 | 1975-1988 |
| 0.8 | 1988-2009 | 1.2 | 1983-2009 | 0.4 | 1988-2009 |
Survival & Stage
Survival
Survival examines how long after diagnosis people live. Cancer survival is measured in a number of different ways depending on the intended purpose. Several examples of survival statistics are listed below. can be calculated by different methods for different purposes. The survival statistics presented here are based on relative survival
A measure of net survival that is calculated by comparing observed (overall) survival with expected survival from a comparable set of people that do not have cancer to measure the excess mortality that is associated with a cancer diagnosis., which measures the survival of the cancer patients in comparison to the general population to estimate the effect of cancer. The overall 5-year relative survival for 2002-2008 from 18 SEER geographic areas was 97.5%. Five-year relative survival by race and sex was: 94.7% for white men; 98.5% for white women; 90.1% for black men; 96.4% for black women.
|
Stage Distribution and 5-year Relative Survival by Stage at Diagnosis for |
||
|
Stage at Diagnosis |
Stage |
5-year |
| Localized (confined to primary site) |
68 |
99.9 |
| Regional (spread to regional lymphnodes) |
25 |
97.1 |
| Distant (cancer has metastasized) |
5 |
53.9 |
| Unknown (unstaged) |
2 |
87.4 |
Lifetime Risk
Based on rates from 2007-2009, 1.03% of men and women born today will be diagnosed with cancer of the thyroid at some time during their lifetime. This number can also be expressed as 1 in 97 men and women will be diagnosed with cancer of the thyroid during their lifetime. These statistics are called the lifetime risk
The probability of developing cancer in the course of one’s lifespan. Lifetime risk may also be discussed in terms of the probability of developing or of dying from cancer. Based on cancer rates from 2007 to 2009, it was estimated that men had about a 45 percent chance of developing cancer in their lifetimes, while women had about a 38 percent chance. of developing cancer. Sometimes it is more useful to look at the probability of developing
The chance that a person will develop cancer in his/her lifetime. cancer of the thyroid between two age groups. For example, 0.24% of men will develop cancer of the thyroid between their 50th and 70th birthdays compared to 0.60% for women.
 Total thyroidectomy. Dr. Kerner will remove the entire gland and the lymph nodes surrounding the gland. Both sections (lobes) of the thyroid gland are usually removed. Additional treatments with thyroid-stimulating hormone (TSH) suppression and radioactive iodine work best when as much of the thyroid is removed as possible.Thyroid lobectomy with or without an isthmectomy. If your thyroid nodules are located in one lobe, Dr. Kerner will remove only that lobe (lobectomy). With an isthmectomy, the narrow band of tissue (isthmus) that connects the two lobes also is removed. After the surgery, your nodule will be examined under a microscope to see whether there are any cancer cells. If there are cancer cells, Dr. Kerner will perform a completion thyroidectomy.
Total thyroidectomy. Dr. Kerner will remove the entire gland and the lymph nodes surrounding the gland. Both sections (lobes) of the thyroid gland are usually removed. Additional treatments with thyroid-stimulating hormone (TSH) suppression and radioactive iodine work best when as much of the thyroid is removed as possible.Thyroid lobectomy with or without an isthmectomy. If your thyroid nodules are located in one lobe, Dr. Kerner will remove only that lobe (lobectomy). With an isthmectomy, the narrow band of tissue (isthmus) that connects the two lobes also is removed. After the surgery, your nodule will be examined under a microscope to see whether there are any cancer cells. If there are cancer cells, Dr. Kerner will perform a completion thyroidectomy.
 Subtotal (near-total) thyroidectomy. Dr. Kerner will remove one complete lobe, the isthmus, and part of the other lobe. This is used for hyperthyroidism caused by Graves’ disease.Dr. Kerner is now doing endoscopic thyroidectomies (Minimally Invasive Thyroidectomy-MIT) using a small incision through which a tiny camera and instruments are passed. He is also utilizing the DaVinci Robot technology for thyroidectomies as well.
Subtotal (near-total) thyroidectomy. Dr. Kerner will remove one complete lobe, the isthmus, and part of the other lobe. This is used for hyperthyroidism caused by Graves’ disease.Dr. Kerner is now doing endoscopic thyroidectomies (Minimally Invasive Thyroidectomy-MIT) using a small incision through which a tiny camera and instruments are passed. He is also utilizing the DaVinci Robot technology for thyroidectomies as well.
Our surgeons combine their vast experience with the latest endoscopic tools to enhance their ability to find the important structures in the neck during surgery, and to assure maximum safety. The thoroughness of MIT is equal to traditional thyroid surgery, and the risks and complications are the same as well. The size of the tumor being removed is a limitation on the size of incision that can be used. One of the most important advantages of MIT is a lot less pain after surgery, and therefore minimal use of pain medications. The reason for the less pain is that the technique is, exactly as the title states, less invasive and thus a lot less traumatic to the tissue. Although the small incision size seems to be a great advantage, and it is, it represents how minimal the trauma to the normal tissue of the neck is in MIT. When the tissue is traumatized less, there is going to be less pain and a lot faster recovery, as well as a much shorter hospital stay. Our patients usually stay overnight after a total thyroidectomy, and some even go home the same day. Patients who have a hemi-thyroidectomy go home on the same day. The blood loss during MIT is usually minimal and we do not use drains.
 Due to the ease of the surgery, limited pain and fast recovery, our patients are extremely happy with their results. There are a few medical conditions and thyroid tumor characteristics that would prevent a patient from being eligible to have MIT, Dr. Kerner will discuss this with you at the time of consultation to see if you qualify.
Due to the ease of the surgery, limited pain and fast recovery, our patients are extremely happy with their results. There are a few medical conditions and thyroid tumor characteristics that would prevent a patient from being eligible to have MIT, Dr. Kerner will discuss this with you at the time of consultation to see if you qualify.
Success of a thyroidectomy to remove thyroid cancer depends on the type of cancer and whether it has spread (metastasized) to other parts of the body. You may need follow-up treatment to help prevent the cancer from returning or to treat cancer that has spread.
Risks
Thyroid surgery is a safe surgery. But there is a risk of complications, including:
Hoarseness and change of voice. The nerves that control your voice can be damaged during thyroid surgery. This is less common if your surgeon has a lot of experience or if you are having a lobectomy rather than a total thyroidectomy.
Hypoparathyroidism can occur if the parathyroid glands are mistakenly removed or damaged during a total thyroidectomy. This is not as common if you have a lobectomy.
If you have a total thyroidectomy, you will develop hypothyroidism and need to take man-made (synthetic) thyroid hormone for the rest of your life. If you have a lobectomy or subtotal thyroidectomy, you may have hypothyroidism and you may need to take thyroid medicine for the rest of your life.
You will most likely be treated with radioactive iodine after surgery for thyroid cancer to make sure that all the thyroid tissue and cancer cells are gone.
You may have a lobectomy, with or without isthmectomy, if your doctor suspects that a nodule may be cancerous. If you do have cancer, a surgeon usually will do a completion thyroidectomy.
After surgery for hyperthyroidism, some people will have low calcium levels and may need to take calcium supplements.
 Surgical workup of a thyroid condition
Surgical workup of a thyroid conditionThe workup of a thyroid mass involves imaging study to determine the size, location, and characteristics of any nodules within the gland. Types of imaging studies include CT or CAT scans, ultrasound, or MRIs. The single most important test is an FNA or fine-needle aspiration biopsy—a safe, relatively painless procedure. With this procedure, a hypodermic needle is passed into the lump, and tissue fluid samples containing cells are taken. Several passes with the needle may be required. Sometimes ultrasound is used to guide the needle into the nodule. There is little pain afterward and very few complications from the procedure. This test gives us more information on the nature of the lump in your thyroid gland and may help to differentiate a benign from a malignant or cancerous thyroid mass.
Thyroid surgery may be required when:
– the fine needle aspiration is reported as indeterminate, suspicious or suggestive of cancer
– imaging shows that nodules have worrisome characteristics or that nodules are getting bigger
– the trachea (windpipe) or esophagus are compressed because one or both lobes are very large
Historically, some thyroid nodules, including some that are malignant, have shown a reduction in size with the administration of thyroid hormone. However, this treatment, known as medical “suppression” therapy, has proven to be an unreliable treatment method.
Choosing a Surgeon
Complications are more likely with surgeons who have less experience performing thyroid surgery, so make sure that your surgeon has extensive experience in thyroid surgery. Dr. Kerner has performed thousands of head and neck surgical procedures. As an attending surgeon at Olive-View UCLA Medical Center, Dr. Kerner was the primary thyroid surgeon from 1995 to 2002 for hundreds of patients in addition to the patients he has cared for in his private practice.
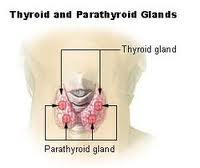
Parathyroid Surgery
 The parathyroid glands are four small glands that are located behind the thyroid gland. They regulate the calcium levels in the blood. Rarely, a gland can grow unregulated which results in too much parathyroid hormone being produced. These are called parathyroid adenomas. This leads to high calcium levels in the blood called hypercalcemia. There are many causes of hypercalcemia; high levels of parathyroid hormone is one of the most common causes of high calcium which is curable with surgery. Dr. Kerner and CalWest surgeons have pioneered minimally invasive surgery for parathyroid gland removal.
The parathyroid glands are four small glands that are located behind the thyroid gland. They regulate the calcium levels in the blood. Rarely, a gland can grow unregulated which results in too much parathyroid hormone being produced. These are called parathyroid adenomas. This leads to high calcium levels in the blood called hypercalcemia. There are many causes of hypercalcemia; high levels of parathyroid hormone is one of the most common causes of high calcium which is curable with surgery. Dr. Kerner and CalWest surgeons have pioneered minimally invasive surgery for parathyroid gland removal.
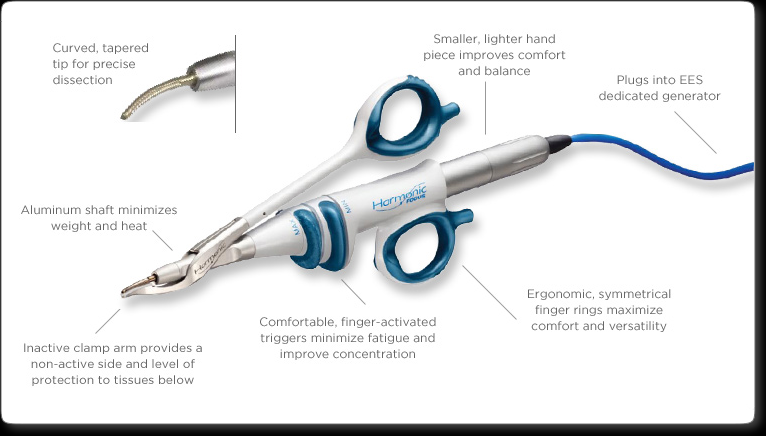
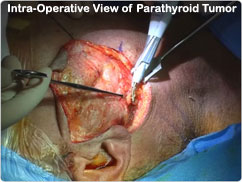
To diagnose hyperparathyroidism, blood tests can identify high levels of both calcium and parathyroid hormone in the blood. A scan called a Sestimibi scan can also be performed which allows anatomic localization of a parathyroid adenoma. (parathyroid pic)
When we see patients in consultation for this condition, we will discuss the surgery at length. We utilize the latest technologies to perform these surgeries. This includes using a nerve monitor to monitor the recurrent laryngeal nerve which can be injured during this surgery. The use of the monitor significantly reduces the chance for damage to the nerve. In addition, we use intraoperative parathyroid hormone assays which allow us to ensure removal of the proper glands by being able to measure the drop in hormone level while the patient is under anesthesia. We also utilize the harmonic scalpel which allows us to perform a minimally invasive surgery through a minimal incision ( usually less than 2 centimeters), and results in faster recovery. The cure rates of surgery are extremely high.






